Overview
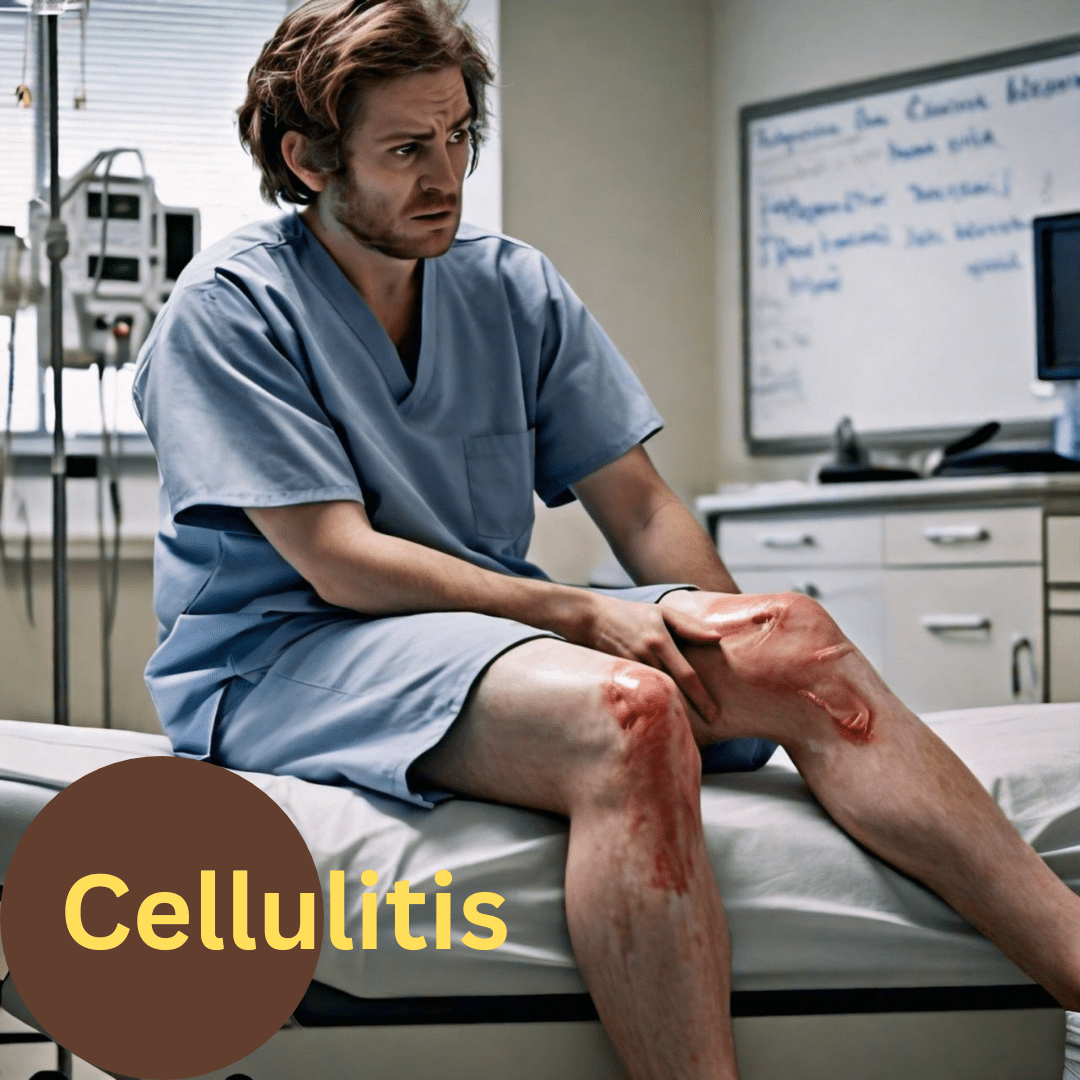
Cellulitis, a bacterial skin infection, characterized by pain and skin discoloration, occurs when bacteria enter the skin through a cut, scrape, or other break in the skin barrier. Without proper treatment, this infection has the potential to spread and result in severe complications.
In the United States alone, there are over 14 million reported cases of cellulitis annually. It can manifest on any part of the body, and when left untreated, it poses significant risks of complications.
While it can affect anyone, those with compromised immune systems or chronic conditions like diabetes are at a higher risk. Recognizing the signs of cellulitis and seeking prompt treatment is essential to prevent complications such as abscess formation or even bloodstream infections.
What is the Most Common Cause of Cellulitis? – 1.
Cellulitis is primarily caused by bacteria, most commonly, Staphylococcus or Streptococcus species. These bacteria can enter the skin through even minor injuries, leading to infection and inflammation.
The skin acts as a vital barrier, shielding the subcutaneous tissue and lymphatic system from normal skin flora and other microbial pathogens. However, when the skin’s integrity is compromised, it creates an opportunity for bacteria, including normal skin flora, to penetrate the dermis and subcutaneous tissue.
This intrusion of bacteria beneath the skin’s surface can trigger an acute superficial infection that affects the deep dermis and subcutaneous tissue, resulting in cellulitis. Typically, cellulitis is caused by the infection with group A beta-hemolytic streptococcus, specifically Streptococcus pyogenes.
Risk Factors
Several factors increase the risk of developing cellulitis, including compromised immune function, skin injuries such as cuts or insect bites, and chronic conditions like diabetes or lymphedema.
Consider this scenario: Individuals with skin conditions such as eczema or athlete’s foot face an elevated risk of cellulitis development. The cracks or fissures created by these conditions serve as entry points for bacteria to infiltrate the skin.
Furthermore, individuals with compromised immune systems are at a heightened risk of cellulitis due to their reduced ability to fend off infections effectively.
What are the Warning Signs of Cellulitis? – 2.
Recognizing the symptoms of cellulitis is crucial for early intervention and preventing complications. Common signs include redness, swelling, warmth, and tenderness in the affected area. In more severe cases, patients may experience fever, chills, and swollen lymph nodes.
Individuals affected by the condition typically exhibit a region of affected skin characterized by poorly defined redness, warmth, swelling, and tenderness upon touch. This erythematous area is often accompanied by constitutional symptoms such as fatigue, malaise, and fever.
Cellulitis has the potential to manifest on various parts of the body, although it predominantly impacts the lower legs and is seldom bilateral. In instances of lower extremity cellulitis, it is crucial to conduct a thorough examination, particularly focusing on the spaces between the toes.
Furthermore, in cases where any extremity is affected, it is imperative to assess sensation and ensure the integrity of pulses to promptly identify signs of compartment syndrome. Additionally, it is important to observe the emergence of vesicles, bullae, or the appearance of Peau d’orange, along with assessing lymphadenopathy.
Ignoring the symptoms of cellulitis can lead to serious complications, including tissue damage, abscess formation, or even sepsis. Prompt treatment with antibiotics is essential to eradicate the infection and prevent its spread.
How to Avoid Cellulitis? – 3.
Preventing cellulitis involves simple yet effective strategies to protect the skin and promote overall health.
Maintaining Good Hygiene
- Regularly wash hands and clean skin thoroughly.
- Keep nails trimmed to prevent scratching and introducing bacteria.
- Moisturize dry skin to prevent cracking and potential entry points for bacteria.
Prompt Wound Care
- Clean and cover any cuts, scrapes, or insect bites promptly.
- Use appropriate wound care products and seek medical attention for deep or infected wounds.
- Avoid picking at scabs or wounds to prevent bacterial entry.
Protecting Skin Integrity
- Wear appropriate protective gear when engaging in activities with a risk of skin injury.
- Use insect repellent to prevent insect bites, which can lead to cellulitis.
- Avoid sharing personal items like towels or razors to minimize the risk of bacterial transmission.
In case a patient experiences skin break, promptly cleanse the area and administer antibiotic ointment. Secure the wound with a bandage and ointment until it has completely healed, ensuring to replace the bandage daily.
Vigilantly monitor the wound for any indications of infection, such as discoloration, discharge, or discomfort, and seek medical attention promptly if any concerning symptoms arise.
In cases where patients display systemic signs of infection, experience treatment failure in outpatient settings, have compromised immune systems, show rapidly advancing erythema, cannot tolerate oral medications, or have cellulitis near or covering an indwelling medical device, hospitalization coupled with systemic antibiotic therapy may become necessary.
How to Heal Cellulitis? – 4.
Treatment for cellulitis typically involves a combination of medical interventions and home care measures:
Medical Interventions
- Antibiotics are the mainstay of treatment for bacterial cellulitis, targeting the specific bacteria causing the infection.
- Pain relievers may be prescribed to alleviate discomfort and inflammation associated with cellulitis.
Home Remedies
- Elevation of the affected limb can help reduce swelling and promote drainage of fluids.
- Warm compresses applied to the affected area can improve blood flow and alleviate pain.
In cases where patients exhibit substantial edema with a known underlying cause, it is imperative to address the root condition effectively. By treating the underlying cause of edema, the goal is to reduce edema levels and mitigate the risk of recurrent cellulitis episodes. Additionally, patients should maintain elevation of the affected area to aid in managing edema and promoting recovery.
Failure to promptly address cellulitis can lead to significant complications, including:
- Sepsis: Bacteria infiltrating the bloodstream, potentially leading to blood poisoning.
- Renal Impairment: Damage to the kidneys due to the spread of infection.
- Leg Ulcers: Chronic wounds that develop on the legs.
Septicemia and renal complications pose life-threatening risks, necessitating urgent hospital intervention and treatment.
Following medical advice and completing the full course of antibiotics is essential to ensure the infection is fully eradicated and reduce the risk of recurrence. If symptoms persist or worsen despite treatment, it is important to seek further medical evaluation.
When to Seek Medical Attention – 5.
While many cases of cellulitis can be managed at home with proper care, certain symptoms warrant immediate medical attention:
- Rapid Spread of Redness: If redness extends beyond the initial site of infection or spreads rapidly, it may indicate a worsening infection.
- Severe Pain: Intense pain, especially if not relieved by over-the-counter pain medication, could signify a deeper or more severe infection.
- Fever and Chills: Persistent fever, chills, or flu-like symptoms may indicate systemic involvement and require urgent medical evaluation.
If a patient experiences any of these symptoms, they should contact their healthcare provider promptly or visit the nearest emergency room for evaluation and treatment.
Final Thoughts
Cellulitis is a common yet potentially serious bacterial skin infection that requires prompt recognition and treatment to prevent complications. While many cases can be managed with prompt medical attention and appropriate treatment, complications can arise, including bloodstream infections (sepsis), tissue damage, abscess formation, or even life-threatening conditions such as septic shock.
It’s essential to recognize the signs and symptoms of this condition and seek medical care if you suspect an infection. Early intervention is key to preventing serious complications and promoting successful treatment. Cellulitis can be serious, particularly if left untreated or if the infection spreads rapidly.
Disclaimer: This blog post is for informational purposes only and should not be construed as medical advice. Always consult with a healthcare professional for specific concerns regarding your health.
References:
- Healthline | Cellulitis: Everything You Need to Know.
- NHS inform | Cellulitis.
- NIH National Library of Medicine | Cellulitis.
FAQs:
- Can cellulitis spread to other parts of the body?
Yes, cellulitis can spread if left untreated, potentially leading to serious complications such as bloodstream infections or abscess formation.
- Is cellulitis contagious?
No, cellulitis itself is not contagious, but the bacteria that cause it can be transmitted through direct contact with infected skin or contaminated objects.
- How long does it take for cellulitis to heal with treatment?
With appropriate treatment, cellulitis symptoms typically improve within a few days. However, it is important to complete the full course of antibiotics as prescribed by your healthcare provider to prevent recurrence.
- Can I prevent cellulitis if I have diabetes?
While individuals with diabetes are at a higher risk of developing cellulitis, practicing good foot care, maintaining stable blood sugar levels, and promptly treating any wounds can help reduce the risk of infection.
Share this valuable information with your friends and family to raise awareness about the importance of cellulitis and skin health. Join the conversation in the comments below!