Introduction
Crohn’s disease is a complex and often misunderstood condition that affects millions of people worldwide. Despite significant advancements in medical research, its causes, treatment options, and long-term management remain challenging for many patients and their families. Whether you or a loved one has been diagnosed, understanding Crohn’s disease is the first step towards living a healthier, more informed life.
Continue reading to explore the key facts about Crohn’s disease, from its underlying causes and symptoms to diagnosis and management strategies. Let’s delve into the details to shed light on this chronic illness.
#1. What is Crohn’s Disease?
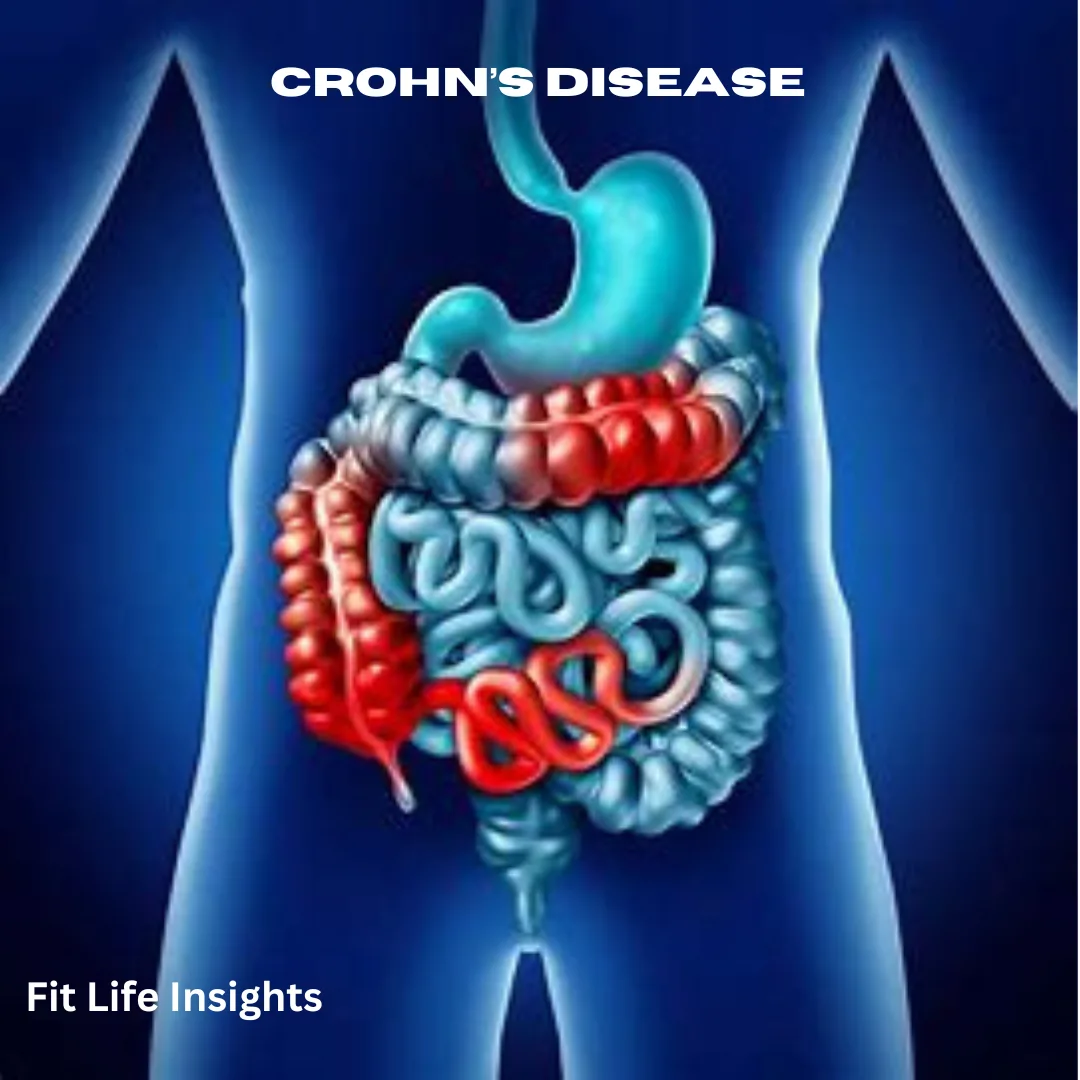
Crohn’s disease is a chronic inflammatory bowel disease (IBD) that causes inflammation anywhere along the gastrointestinal (GI) tract, from the mouth to the anus. However, it commonly affects the small intestine and the beginning of the large intestine. The inflammation can involve different layers of the digestive tract, leading to severe discomfort and complications.
While Crohn’s disease can develop at any age, it is most often diagnosed in young adults between the ages of 15 and 35. Symptoms can vary widely from person to person, making the condition difficult to diagnose early on. Additionally, Crohn’s is characterized by alternating periods of flare-ups and remission, further complicating its course.
Unlike some other digestive diseases, Crohn’s disease is not caused by dietary choices alone. Instead, it is believed to result from a combination of genetic, environmental, and immune system factors.
#2. Causes of Crohn’s Disease
The exact cause of Crohn’s disease remains unknown, but research highlights a combination of contributing factors:
- Immune System Dysfunction: Crohn’s disease may occur when the immune system mistakenly attacks healthy cells in the gastrointestinal tract, leading to its inflammation.
- Genetic Predisposition: Individuals with a family history of Crohn’s are at a higher risk of developing the disease. Certain genetic mutations have been linked to its occurrence.
- Environmental Triggers: Factors such as smoking, infections, and diets high in processed foods may trigger or worsen symptoms in susceptible individuals.
While these factors increase the likelihood of developing Crohn’s, no single cause has been identified. It is this combination of genetics, immune dysfunction, and environmental triggers that make the disease so difficult to predict or prevent.
#3. Recognizing the Symptoms of Crohn’s Disease
Crohn’s disease symptoms vary depending on the severity and location of inflammation within the GI tract. Common signs and symptoms include:
- Persistent Diarrhea: Loose, watery stools are one of the most frequent symptoms.
- Abdominal Pain and Cramping: Inflammation can cause severe pain, often in the lower-right part of the abdomen.
- Fatigue: Chronic inflammation and nutrient deficiencies can result in extreme tiredness.
- Weight Loss and Malnutrition: Reduced appetite and impaired nutrient absorption contribute to unintended weight loss.
- Fever: Inflammation may lead to intermittent fevers.
In addition to these common symptoms, some individuals may develop complications such as bowel obstruction, ulcers, or fistulas. Symptoms often worsen during flare-ups, which may occur unpredictably.
Extraintestinal Symptoms: Crohn’s disease can also affect other parts of the body, causing issues such as joint pain, skin rashes, and eye inflammation.
#4. How is Crohn’s Disease Diagnosed?
Diagnosing Crohn’s disease involves multiple steps due to its wide-ranging symptoms. Early and accurate diagnosis is critical for effective treatment. Doctors use the following methods:
- Medical History and Physical Exam: Your healthcare provider will discuss your symptoms, family history, and lifestyle habits.
- Lab Tests: Blood tests can identify anemia (low red blood cells) or elevated inflammatory markers. Stool tests may also be used to rule out infections.
- Endoscopy and Colonoscopy: These procedures allow doctors to view the digestive tract and obtain tissue samples of biopsy.
- Imaging Tests: CT scans, MRI, X-rays may help locate areas of inflammation or complications such as strictures and fistulas.
Given the overlap between Crohn’s disease and other gastrointestinal conditions like ulcerative colitis, accurate diagnosis often takes time. Regular monitoring and follow-ups are essential for managing symptoms effectively.
#5. Complications of Crohn’s Disease: When Symptoms Worsen
If left untreated or poorly managed, Crohn’s disease can lead to serious complications. Some of the most concerning include:
- Bowel Obstruction: Chronic inflammation can thicken the walls of the intestine, narrowing the passage and blocking bowel movement.
- Fistulas: These abnormal connections between the intestine and other organs can cause infections and require surgical intervention.
- Ulcers: Open sores can develop in the digestive tract, mouth, or surrounding tissues.
- Malnutrition: Poor nutrient absorption can lead to vitamin and mineral deficiencies, causing anemia and weak bones.
- Colon Cancer: Prolonged inflammation increases the risk of colon cancer, particularly in patients with Crohn’s disease of the large intestine.
Understanding these complications highlights the importance of timely intervention and long-term care for individuals living with Crohn’s disease.
#6. Treatment Options for Crohn’s Disease
While there is no cure for Crohn’s disease, various treatments can help manage symptoms, reduce inflammation, and prevent complications. Treatment plans are often tailored to individual needs and may include:
- Medications
- Anti-inflammatory drugs: Corticosteroids and aminosalicylates help reduce inflammation.
- Immunosuppressants: These drugs suppress the immune system to prevent it from attacking the GI tract.
- Biologics: Targeted therapies block specific proteins causing inflammation.
- Antibiotics: These can treat infections or reduce harmful bacteria in the gut.
- Nutritional Therapy
- Specialized diets or liquid nutrition may help reduce inflammation during flare-ups.
- Nutrient supplements may address deficiencies caused by malabsorption.
- Surgery
In cases where medications and dietary changes fail, surgery may be necessary to remove damaged sections of the digestive tract or repair complications like fistulas.
#7. Lifestyle Management: Living Well with Crohn’s Disease
Managing Crohn’s disease requires a comprehensive approach that includes lifestyle modifications to reduce symptoms and improve quality of life. Here are some tips:
- Adopt a Healthy Diet: Eat smaller, more frequent meals. Avoid trigger foods such as spicy, fatty, or high-fiber foods.
- Stay Hydrated: Drink plenty of water to prevent dehydration caused by diarrhea.
- Quit Smoking: Smoking worsens inflammation and increases the risk of flare-ups.
- Manage Stress: Stress can exacerbate symptoms, so practice relaxation techniques like yoga or meditation.
- Exercise Regularly: Moderate physical activity can boost energy levels and overall health.
With the right combination of medical care, healthy habits, and emotional support, individuals with Crohn’s disease can lead fulfilling lives.
Closing Thoughts
Crohn’s disease can feel overwhelming, but knowledge is power. By understanding its causes, symptoms, and treatment options, you can take charge of your health and build a better future. While the journey may be challenging, ongoing advancements in medicine and lifestyle management offer hope for living well with Crohn’s disease.
Remember, seeking professional medical advice is crucial for effective management. Surround yourself with a supportive community, and take proactive steps towards wellness. Living with Crohn’s disease is a journey, but with the right tools, it is one you can navigate successfully.
Disclaimer: This blog post is for informational purposes only and does not constitute medical advice. Always consult a healthcare professional for diagnosis and treatment.